HIV and COVID-19: Lower CD4 cell counts linked to serious COVID-related outcomes

Certain factors increase the risk of serious COVID-19-related outcomes- having HIV is one of them. Our analysis shows that uncontrolled HIV based on low CD4 cell counts is linked with a higher risk of serious outcomes.
Authors
Chanie Suttner (Actuary at Discovery Health); Michael Cohen (Actuary at Discovery Health); Shirley Collie (Chief Research Actuary at Discovery Health)
Investigating the risk of serious COVID-19 outcomes for people with HIV
Data reported to the WHO Global Clinical Platform for COVID-19 from 37 countries show that HIV infection significantly increases the risk of severe illness and in-hospital mortality when people get COVID-19.1
To learn more about the links between HIV and COVID-19 outcomes, we analysed medical scheme member data over 36 months (between 1 March 2020 and 31 March 2023).
Our sample group
This analysis is based on a sample group of 638,689 members across all medical schemes administered by Discovery Health who had been diagnosed with COVID-19 at least once.
In our sample, 15,190 (2.4%) members were registered for HIV benefits through the Chronic Illness Benefit (CIB) programme. In total, 77,086 members were registered as having HIV at March 2023, of which 19.7% had been diagnosed with COVID-19 at least once.
Our methodology
To carry out this analysis, we looked at risk factors and COVID-19 outcomes among medical scheme members.
The risk factors we considered were:
- Whether members were registered for HIV benefits or not
- For members registered for HIV benefits, their CD4 cell count.
- CD4 cells are (also known as CD4+ T cells) are white blood cells that help fight infection2 . A CD4 cell count (measured as the number of cells per cubic millilitre of blood pr cells/mm3) is used to monitor the immune system function of people with HIV.
To understand the association between these risk factors and members' health outcomes, we also considered the impact of members' demographics (such as age and sex) and clinical profiles.
Confounders (also called confounding variables) are factors that affect both risk factors and outcomes.
Confounders that we considered were:
- Member's age and sex
- Certain co-morbidities that affect the risk of adverse outcomes for COVID-19 for example, asthma, chronic kidney failure, cancer, diabetes, hypercholesterolaemia high cholesterol, hypertension (high blood pressure), and coronary heart disease.
- Province that the member lives in
- COVID-19 wave in which the member contracted the illness
- Number of times the member was infected with COVID-19
- Member's COVID-19 vaccination status
We considered the following to be severe COVID-19 outcomes:
- Hospital admissions (being admitted to hospital because of COVID-19)
- Mortality rates (deaths related to COVID-19)
The details of our analysis and findings are set out below.
Heightened risk of COVID-19-related admission and mortality among members registered for HIV benefits (HIV positive people)
What we analysed
To see how being HIV positive might COVID-19-related outcomes, we assessed the relative risk of having serious COVID -19 outcomes, after a member's most recent COVID-19 infection. We did this for, members who were and were not registered for HIV benefits
Within the sample group:
- There were 69,017 hospital admissions (10.4%) and 15,360 deaths (2.3%) relating to COVID-19 for all members
- There were 2,515 hospital admissions (16.6%) and 533 deaths (3.5%) relating to COVID-19 for members registered for HIV benefits
Findings from this analysis
Finding 1: Members registered for HIV benefits had a higher risk of COVID-19-related hospital admissions and death.
When we compared the COVID-19-related outcomes for members registered for HIV benefits versus those not registered for HIV benefits, we found that:
- Members registered for HIV benefits had a 1.6-times higher risk of being admitted to hospital for COVID-19.
- Members registered for HIV benefits had a 2.3-times time higher risk of death from COVID-19.
These results were statistically significant at a 95% confidence level (see Figure 1)
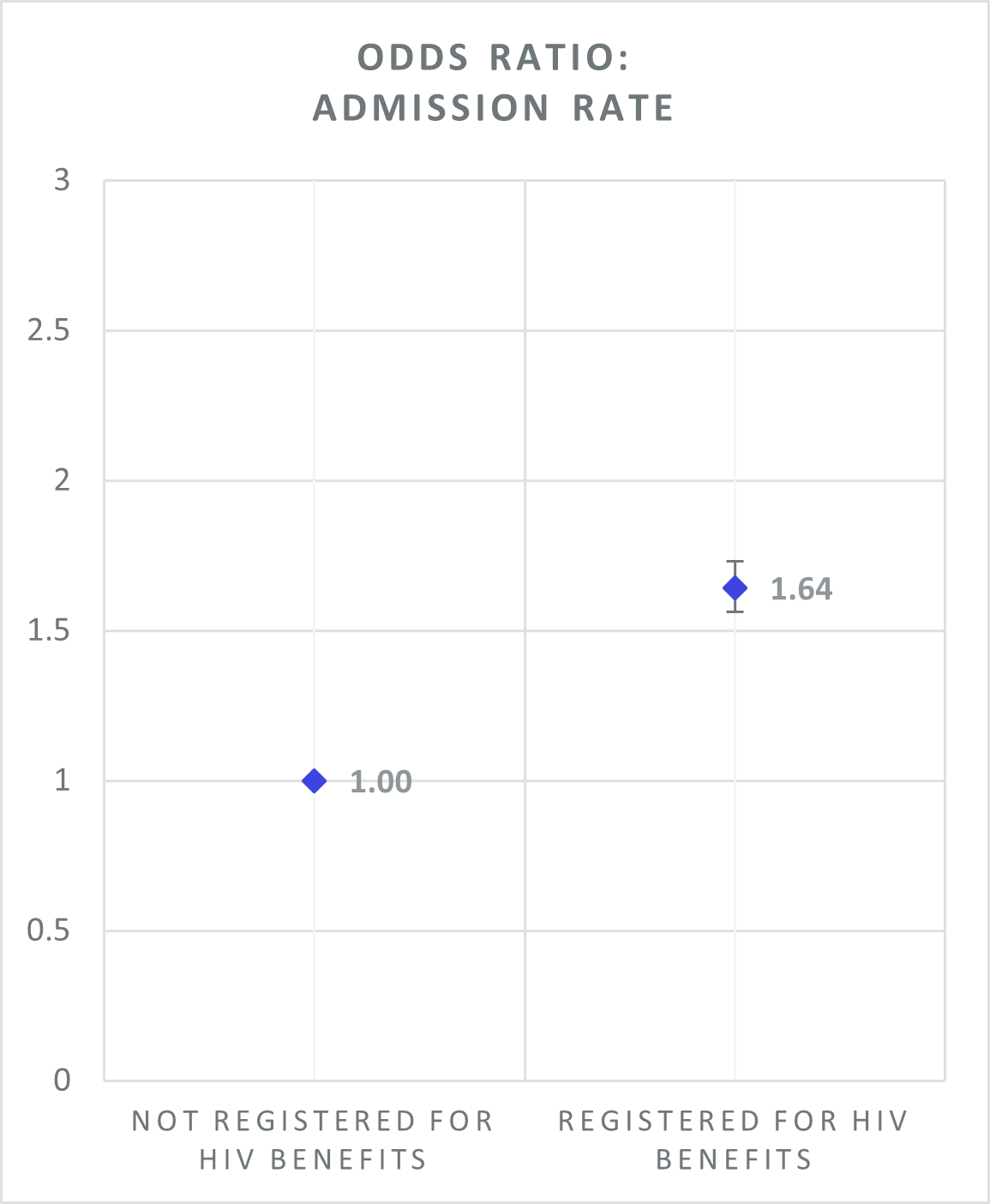
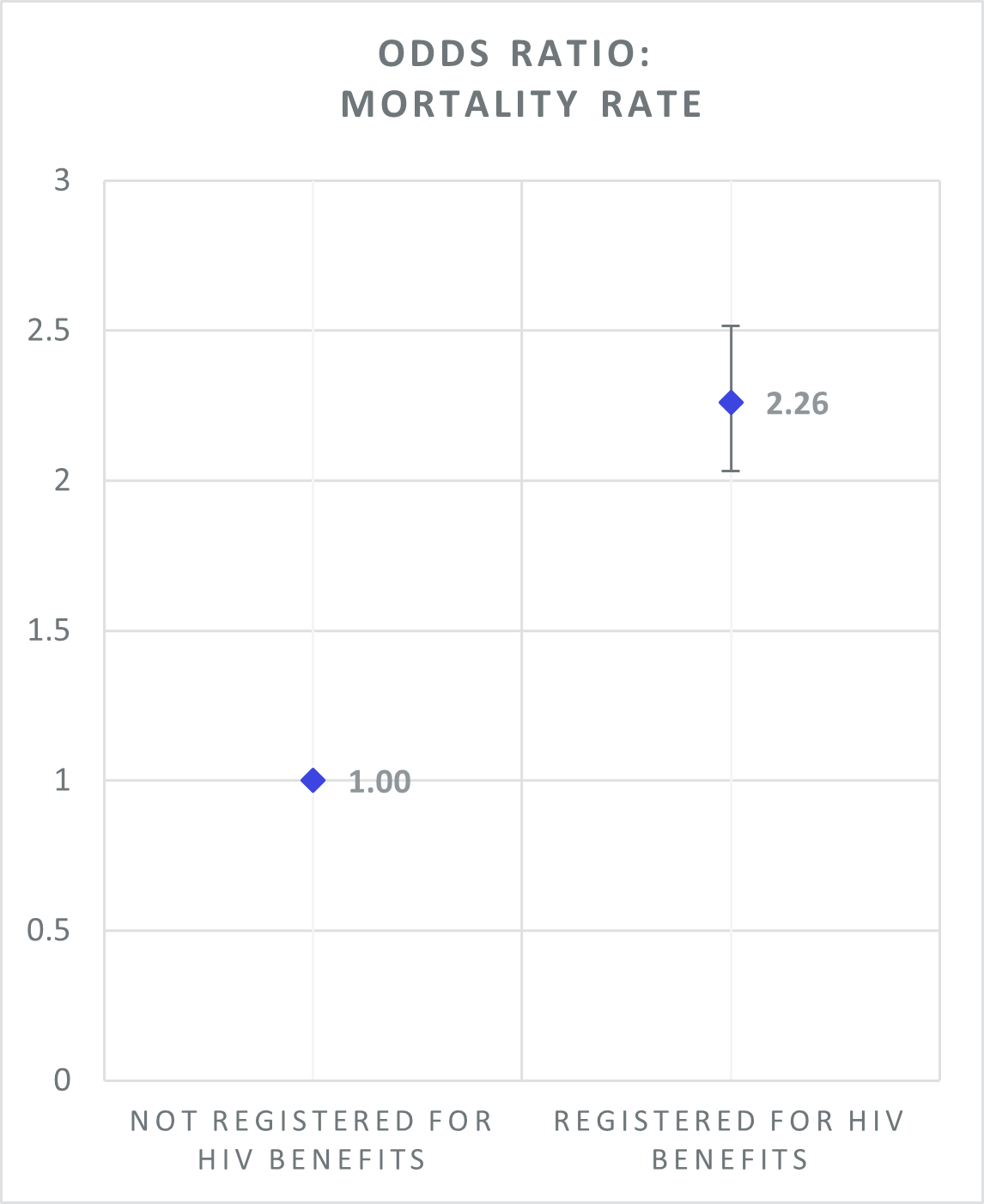
Figure 1: Odds ratios for COVID-19-related hospital admissions and mortality for members registered for HIV benefits relative to members not registered for HIV benefits. (Members who are not registered are included in the baseline population, depicted with a value of 1 against which the admission and mortality risks of members registered for HIV benefits can be compared).
Heightened risk of COVID-related hospital admissions and mortality linked to low CD4 cell counts
What we analysed
To examine the degree to which COVID-related outcomes are related to the severity of the HIV infection among members registered for HIV benefits, we analysed CD4 cell count test results in the 12 months before member's last positive COVID-19 infection.
CD4 cell count normal range is 500 to 1500 cell/mm^3. If a patient is left untreated, levels can drop below 200 cells/mm^3, which is one indication for the diagnosis of AIDS3.
In our sample:
- 77% of the sample group who were included in the analysis had a CD4 cell count test result.
- 23% of members had not done a test to measure CD4 cell count in the twelve months before they were diagnosed with COVID-19, so there were no results available
For those who had test results:
- 6% of members had a CD4 cell count of less than 200 cell/mm3
- 20% of members had a CD4 cell count between 200 and 500 cell/mm3
- 50% of members had a CD4 cell count of greater than 500 cell/mm3
- 23% of members had not done a test to measure CD4 cell count in the twelve months before they were diagnosed with COVID-19, so there were no results available
The distribution of CD4 cell counts for members within 12 months prior to their last COVID-19 infection is shown in Figure 2 below.
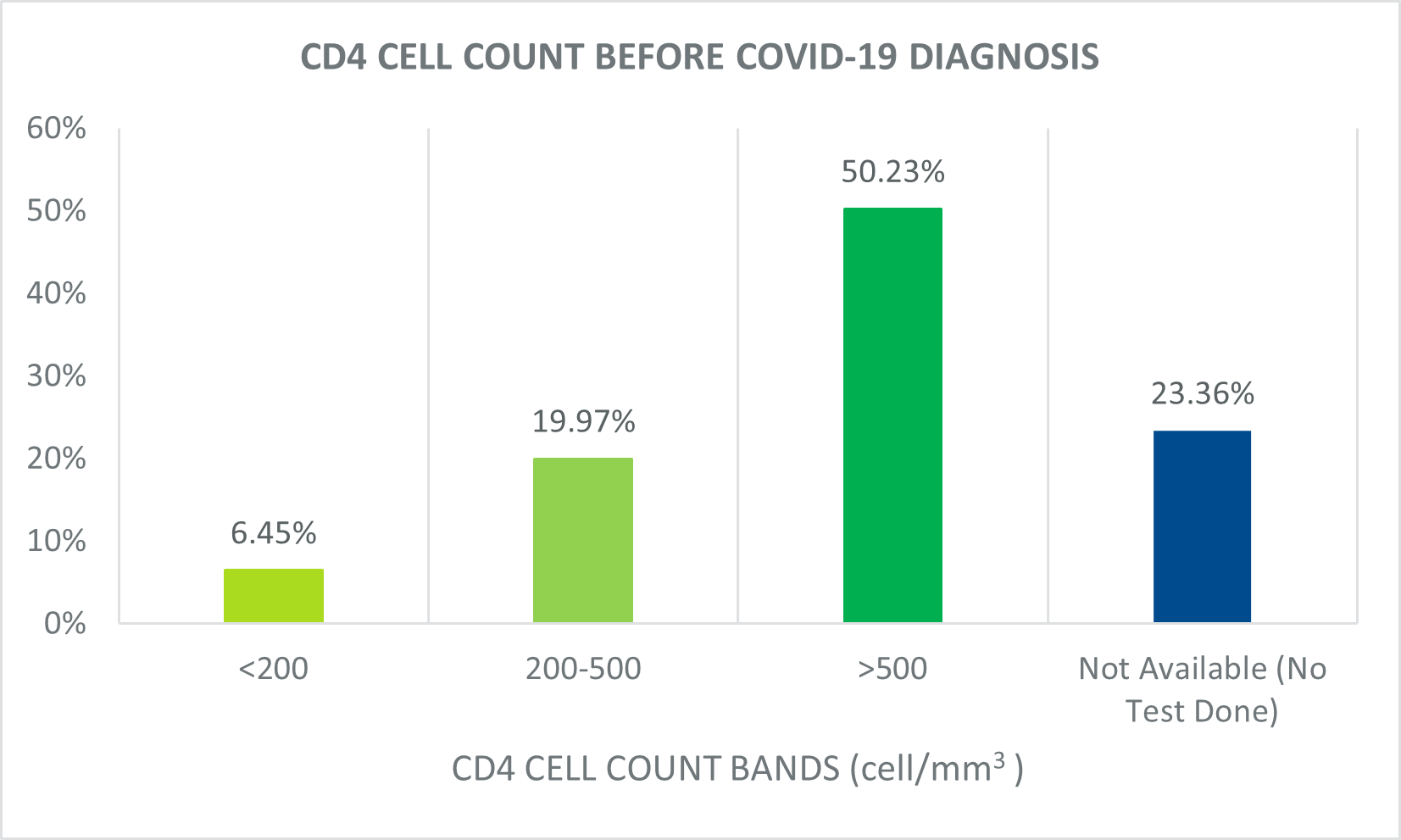
Figure 2: Sample group's CD4 cell count results before most recent positive COVID-19 diagnosis
Findings from this analysis
Finding 2: Members registered for HIV benefits who had low CD4 cell counts (<200 cell/mm3) had a higher risk of COVID-related hospital admission and death than those members with higher CD4 cell counts.
When we compared COVID-related outcomes in members who had CD4 cell count of <200 cell/mm3 and members who had a CD4 cell count of >500 cell/mm3, we found that:
- Members who had CD4 cell count of <200 cell/mm3 had a 3.5-times higher risk of being admitted to hospital for COVID-19
- Members who had CD4 cell count of <200 cell/mm3 had a 4.2-times higher risk of death from COVID-19
This shows that members with potentially untreated HIV (CD4 cell count of <200 cell/mm3,) are more at risk of severe COVID-19 outcomes (admissions and deaths) than those with a CD4 cell count within a normal range (CD4 cell count normal range is 500 cell/mm3).
And, when we compared COVID-related outcomes of members who had CD4 cell counts of between 200 to 500cell/mm3 to those who had CD4 cell counts of >500 cell/mm3, we found that:
- Members who had a CD4 cell count of between 200 to 500cell/mm3 had a 1.3-times higher risk of being admitted to hospital for COVID-19
- Members who had CD4 cell count of between 200 to 500cell/mm3 had a 1.4 times higher risk of death from COVID-19
Members with a CD4 cell count of between 200 to 500 cell/mm3 had a higher risk of COVID related admission and death than those with an in-range CD4 cell count (1.3 and 1.4 times higher risk of admission and death respectively). Yet their risk was lower than the risk faced by those members with CD4 cell count of <200 cell/ mm3 relative to those with an in-range CD4 cell count (3.5 and 4.2 times higher risk of admission and death from COVID-19 respectively).
This finding may indicate that the higher the level of CD4 cell counts, the lower the risk of severe COVID-19 related outcomes.
These results were statistically significant at a 95% confidence level.
This can be seen in Figures 3 and 4 below.
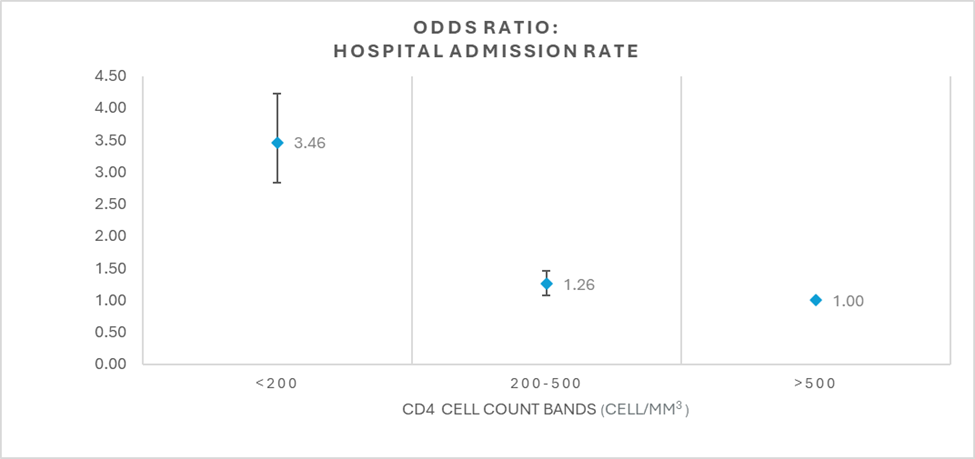
Figure 3: Odds ratios for COVID-19-related hospital admissions by CD4 cell count band results where in-range the CD4 cell counts are (>500 cell/mm3). Members registered for HIV benefits with a CD4 cell count within normal range are included in the baseline population, depicted with a value of 1, against which the admission risks of members registered for HIV benefits with lower CD4 cell count bands can be compared.
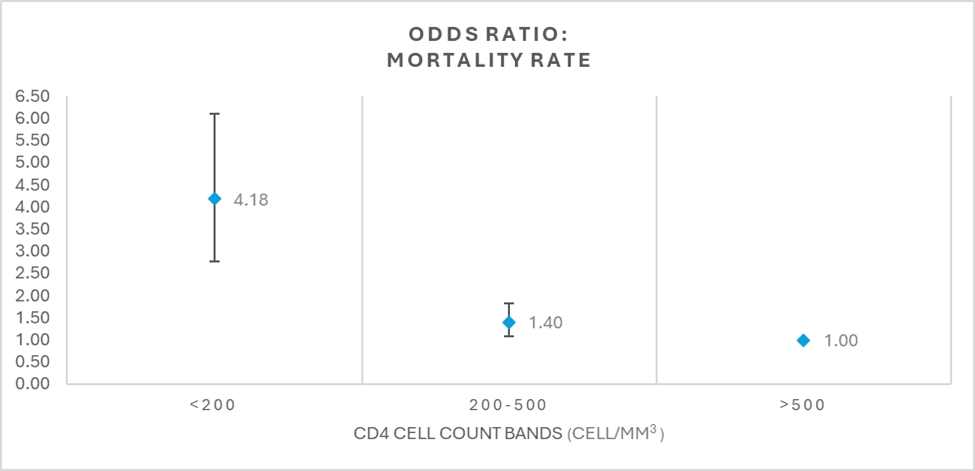
Figure 4: Odds ratios for COVID-19-related mortality by CD4 cell count band results where in-range CD4 cell counts are >500 cell/mm3. Members registered for HIV benefits with a CD4 cell count within normal range are included in the baseline population, depicted with a value of 1, against which the mortality risks of members registered for HIV benefits with lower CD4 cell count bands can be compared
Summary of insights
Our results show that Discovery Health administered medical scheme members who are registered for HIV benefits are at an increased risk of severe COVID-19 outcomes compared to those members who are not HIV registered.
Furthermore, among members registered for HIV benefits, it is those who have lower CD4 cell counts who are at increased risk of severe COVID-19 outcomes. This, compared to members who have higher CD4 cell counts and particularly when compared to those members who are well managed with CD4 cell counts >500 cell/mm3
References
1WHO warns that HIV infection increases risk of severe and critical COVID-19
3Acquired Immune Deficiency Syndrome CD4+ Count
Acknowledgements
We would like to acknowledge Marothi Peter Letsoalo (MSc (GradStat)) and Vivek Naranbhai (MBCHB, PhD), our collaborators at the Centre for the AIDS Programme of Research in South Africa (CAPRISA), for their invaluable assistance in carrying out this analysis and in delivering its findings.
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and to obtain any further context required.
Did you find this post interesting?
Please visit our Discovery Health Insights Hub for a range of analyses and insights shared by our Discovery Health Intelligence Team over the past three and a half years and spanning a variety of health-related themes. All of our COVID-related analyses are posted under our "COVID-19 Insights" pillar.
All information shared on this page is based on perspectives gained from analysis of figures and trends emanating from discovery health's data pool. The analysis, which is conducted by discovery health's actuarial and data scientist team, aims to encourage industry dialogue. This content is shared for educational and informational purposes only. It does not constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions.

Long COVID symptoms, impact on carrying out daily activities: Survey of just over 7,000 medical scheme members reveals key insights
16 June 2022
Authors: Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health), Lizelle Steenkamp (Senior Healthcare Statistician, Discovery Health), Lebohang Radebe (Data Scientist, Discovery Health), Dr Smybinn Mathews (Clinician, Discovery Health) and Dr Dave Jacobs (Senior Clinician and Clinical Classification System Architect, Discovery Health)